-
-
-
siddharthshroff92@gmail.com
Anugrah Clinic, Hiranandani Meadows, Thane 400610.
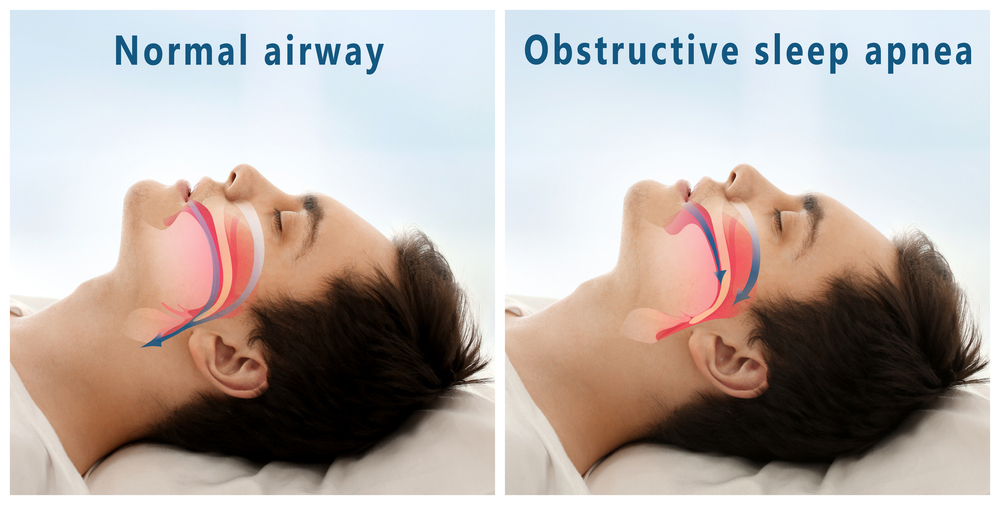
Sleep apnoea is a serious sleep disorder in which breathing repeatedly stops and starts during sleep. The most common form, obstructive sleep apnoea (OSA), occurs when the muscles of the throat relax excessively, causing a temporary blockage of the upper airway. This leads to reduced oxygen supply, interrupted sleep, loud snoring, gasping episodes, and daytime fatigue. Untreated sleep apnoea increases the risk of high blood pressure, heart disease, stroke, diabetes, and impaired cognitive function.
While lifestyle modifications, weight management, and continuous positive airway pressure (CPAP) therapy are first-line treatments, certain patients may not tolerate or benefit from these methods. In such cases, head and neck surgeries can offer a long-term solution by physically correcting the structural problems causing airway obstruction.
Surgeries for sleep apnoea are often performed by ENT (Ear, Nose, and Throat) specialists or head and neck surgeons with advanced training. These specialists evaluate the entire upper airway using sleep studies, endoscopic examinations, and imaging to determine the exact site(s) of obstruction.
The goal of surgery is to reduce apnoea episodes, improve oxygen levels, restore restful sleep, and enhance overall quality of life. Recovery time varies depending on the procedure, ranging from a few days to several weeks. Post-operative care may include pain management, dietary modifications, voice rest, and follow-up sleep studies to assess improvement.
For individuals whose sleep apnoea is caused by anatomical obstructions, head and neck surgeries can be life-changing. By restoring normal breathing patterns during sleep, these procedures not only reduce health risks but also improve energy levels, mood, and cognitive performance. Early diagnosis and consultation with a qualified specialist are key to achieving the best possible outcomes.